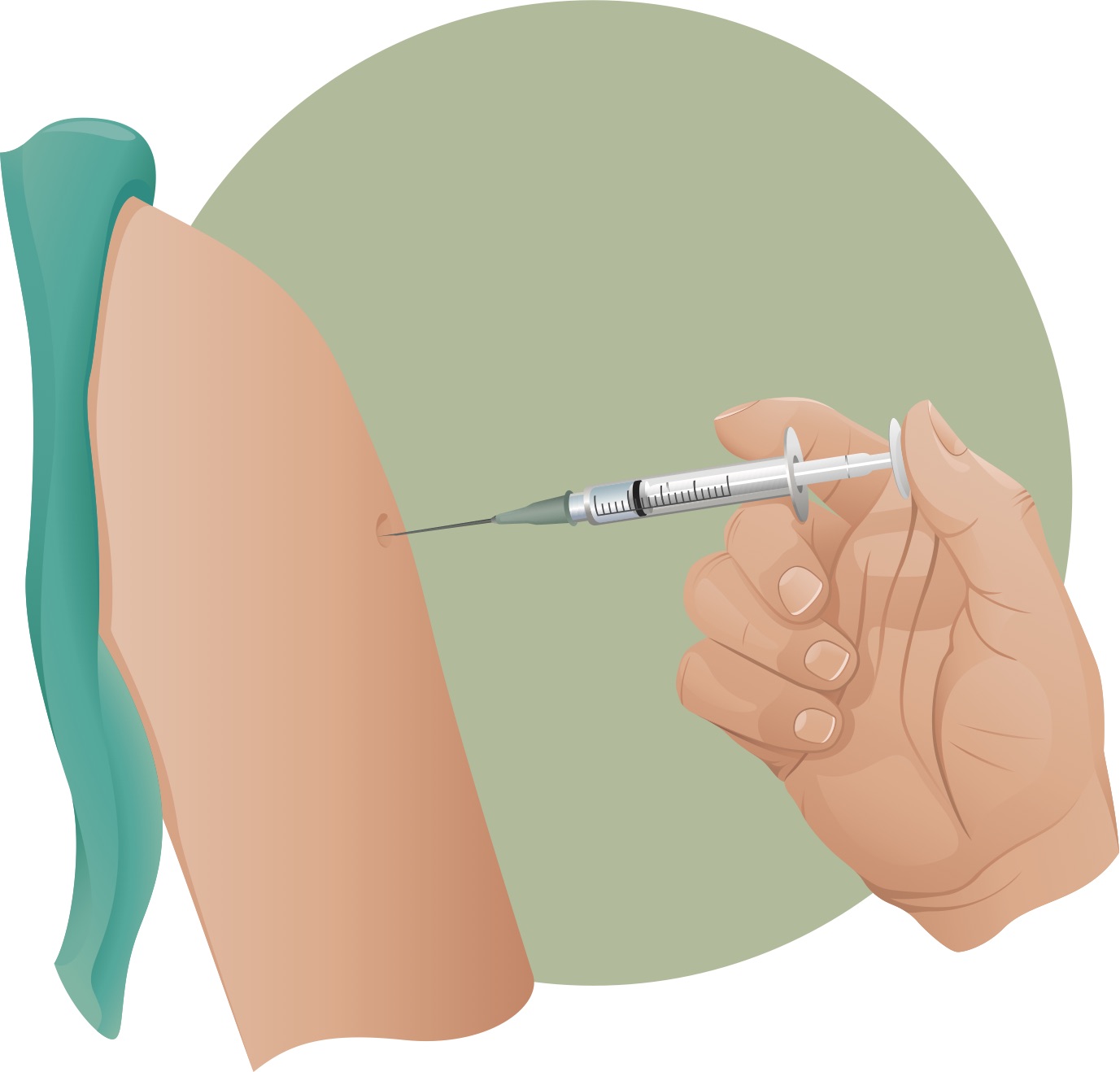
Drug and biological product administration via intramuscular injections using hypodermic needles has been a common medical practice for several centuries and is not going anywhere soon—from vaccines, antibiotics and insulin to an experimental injectable male contraceptive in development.1 The main issue with intramuscular injections is that if the hypodermic needle containing the drug or biological is injected incorrectly into a muscle or another part of the body, it could cause serious harm.
Hitting the Sweet Spot
Once administered exclusively by physicians, nurses began to take on the duties of giving intramuscular injections starting in the 1960s as children were being injected with an increasing number of vaccines. Normally, injection sites are focused on muscle areas and, depending on the formulation, the drug or biological is then absorbed into the bloodstream quickly or gradually.
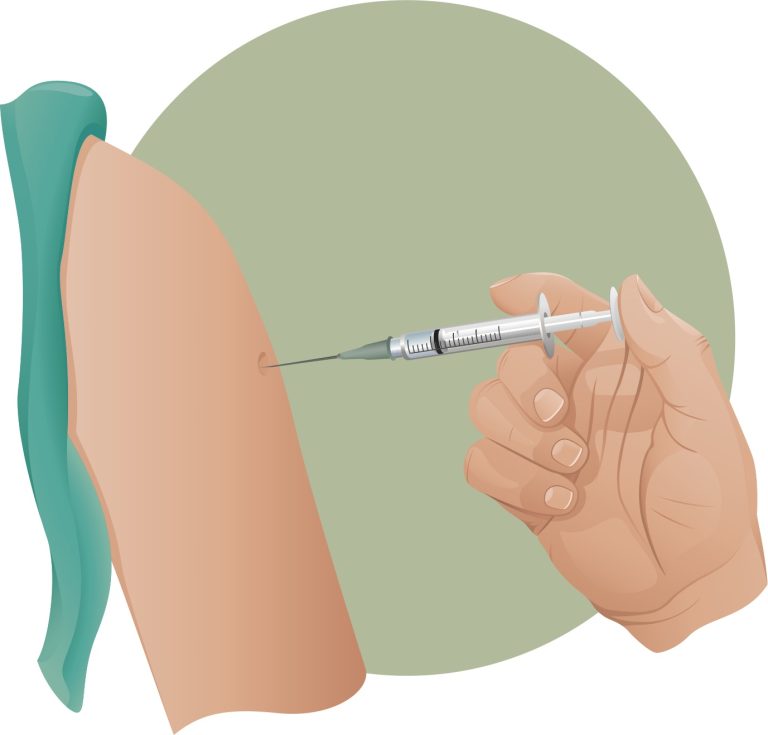
Doctors and nurses administer vaccines in four different muscular areas: deltoid muscle of the arm, vastus lateralis muscle of the thigh, ventrogluteal muscle of the hip and the dorsogluteal muscle of the buttocks.2 And while it does depend on the agent injected, specific injection sites can decrease the risk of injection-related injuries. The first rule of thumb is that shorter, higher gauge needles minimize complications.
Secondly, guidelines recommend administering shots in the upper outer quadrant of a person’s buttocks: the ventrogluteal muscle of the hip. It provides the greatest thickness of the gluteal muscle and is free of penetrating nerves and blood vessels. It also has a narrower layer of fat.
The dorsogluteal muscle of the buttocks, on the other hand, is linked with a higher risk of sciatic nerve injury (lower back, hip, back of leg). The deltoid site is commonly used in outpatient settings, however there is a need for caution because of the close proximity of the bone, radial nerve and brachial (shoulder to elbow) artery.3
Nerve Damage Resulting From Gluteal Intramuscular Injections
Intramuscular injections resulting in nerve damage are fairly common, especially in children. According to a 2000 retrospective study, 86.2 percent of study subjects experienced gluteal sciatic nerve injuries caused by intramuscular injection.4
A review of claims in New Zealand’s Accident Compensation Coorporatoin between 2005 and 2008 reveals that eight claims were for sciatic nerve injury as a result of intramuscular injection. A literature review in the same study identified 17 reports of 1506 patients—most of which were children—with sciatic nerve injury from intramuscular injections.5
A 2006 case study presented a 25-year-old-male who developed a painful, swollen left leg after several left gluteal intramuscular injections (for indications and drugs unknown). Further analysis revealed marked muscle wasting consistent with a partial sciatic nerve injury.6
Nurses Commonly Using Wrong Injection Site
Despite recommendations for using the ventrogluteal (hip) site, there are discrepancies within nursing textbooks and very few nurses choose the safest injection site. According to a 2007 survey among registered nurses from outpatient settings, 99 percent reported using the dorsogluteal (buttocks) site versus 9 percent using the ventrogluteal site.7
A larger 2011 Canadian study showed similar findings. While 71 percent of hospital nurses most often gave intramuscular injections in the dorsogluteal site, only 14 percent used the ventrogluteal site.
Further, more than one in four nurses using the dorsogluteal site were unaware of the potential nerve damage risk linked with that spot. However, 74 percent of the nurses using the dorsogluteal site reported nerve injury as a complication in their patients. Only 15 percent of the nurses based their decision on nursing literature recommendations; 85 percent said their comfort level influenced their site selection.
The findings also revealed that younger, newer nurses (aged 20-24 years) were significantly more likely to follow the site injection recommendations as compared with their older, experienced colleagues (aged 40 years or older). All the respondents had been working in the nursing field for more than 10 years.8 9
No injection site may be without hazard, but the data indicate there is an unused best practice. “The implications for nurses include the need to learn and practice safe injection technique,” the researchers wrote. “Proper training and an anatomical understanding of the sciatic nerve course are essential.”10
References:
1 Behre HM, Zitzmann RA, Anderson DJ, et al. Efficacy and Safety of an Injectable Combination Hormonal Contraceptive for Men. The Journal of Clinical Endocrinology & Metabolism Oct. 27, 2016.
2 Cafasso J. What Are Intramuscular Injections? Healthline Oct. 5, 2015.
3 Omoigui S, Ogbechie C and Fadare A. Reinventing IM and Procedural Injections: The Sota Omoigui Short Needle Technique. Practical Pain Management Feb. 9, 2016.
4 Huang Y, Yan Q, and Lei W. Gluteal sciatic nerve injury and its treatment. Chinese Journal of Reparative and Reconstructive Surgery 2000;14:83-86
5 Mishra P and Stringer MD. Sciatic nerve injury from intramuscular injection: a persistent and global problem. International Journal of Clinical Practice July 27, 2010.
6 Ramtahal J, Ramlakham S and Singh K. Sciatic nerve injury following intramuscular injection: a case report and review of the literature. Journal of Neuroscience Nursing 2006;38:238-40.
7 Floyd S and Meyer A. Intramuscular injections—What’s best practice? Kai Tiaki Nursing New Zealand 2007;13:20-22.
8 Walsh L and Brophy K. Staff nurses’ sites of choice for administering intramuscular injections to adult patients in the acute care setting. Journal of Advance Nursing 2011;67:1034-40.
9 Wiley-Blackwell. Most nurses don’t use recommended intramuscular injection site despite potential risks, study finds. Science Daily May 9, 2011.
10 See Footnote 6.












42 Responses
I see plenty of nurses smoking cigarettes outside my local hospital buildings. It isn’t surprising they don’t know (and likely don’t care to know) about safer injection sites. After all, most in the ‘health’ field don’t know the first thing about vaccines, so why would they wish to know about injection sites?
What’s smoking have to do with giving a shot? You sound uneducated.
My son has damage to his right hip
In regards to being given a shot to the hip. She but his sciatica nerve and hurts all the time. Some days all he can do is limp. Is there someone that I can talk to regarding this issue?
Debra, My name is Judy Reid. I was also given a hip shot and have been in pain every since. The pain is in my hip and runs down my leg; I’ve even started to swell in those same areas. Where are you from? I would like to talk to you on the phone. My number is 856-506-5249. I live in the State of Mississippi. I don’t want to talk much about this subject on the internet. Please call me and if i can’t talk, i will set a time to call you back.
Thank you Debra
Hello,
Against my better judgment I got a shot of antibiotics in my right butt cheek on Tuesday last week. Thursday over night I began to have an ache in my hip. By Thursday afternoon I could not walk without pain, sit or lay down. I thought my hip was out of place and went to the chiropractor. Small amount of reliefs for a few hours and still tons of pain.
Does this sound possibly to be related to the injection. Now I’m scared.
What does their smoking have to do with whether or not they don’t know or don’t care about safer injection sites? You are correct in your remark about most in the health field not knowing about vaccines, but whether or not they wish to know about injection sites is most likely not their preference, but their ignorance of there being a best site for injections.
I had an injection into my left forearm in Feb. 2001, that has done considerable damage to my body (the contents of the injection were the issue, and also that it was injected into a vessel). The response was instant, I could not talk, walked out of the office like a zombie, had tachycardia 10 minutes later while driving on a freeway. This so called nurse did it with intent because I irritated her by asking too many questions, at a Public Health Dept in San Diego. The manufacturer of the product representative told me I was given an overdose. It was an inch of fluid in the needle, I watched, and when I protested that it was too much she jammed it in hard. I had no voice as it was very difficult to speak and walk for years.
Yet no doctor wants to deal with my issues. No attorney wanted to deal with this sort of case. Still have pain in the site on left arm, plus whole body, especially head pain involving ears.
And yes I do try to avoid doctors by taking good care of what I have left of myself.
I’ve had very similar issue. If you have interest in exchanging information, let me know by text and we can exchange contact info.
I’ve have great legal representation on my impending complaint.
And I’ve gotten references to the top 3 doctors in the country to address recovery.
Thanks
Maria
Please email me the drs you have information on regarding IM gluteal injections.
Hi Maria
I had a similar experience, and the doctor was irritated because I had complained about the previous doctor because that doctor doubted my regular Neurologist’s (who was on maternity leave) decision to give me the series of Botox injections when I did not have spastiscity on that arm.
I live in San Diego, and would like to share info. I think I might have nerve damage. The doctor refused to give me a gown, and told me to roll up my long sleeve, and although I protested, he went on and gave me the injection anyway. The was standing on my left side and gave the injection 30 degree inclined, from the top of my arm. The area was squished and the injection was administered high on my shoulder. Now I have tremors like seizures of my left hand, in the mornings I need help to get up, I feel electrical shocks and numbness. I wake up several times in the night and feel very tired in the morning. My primary doctor said I have Frozen Shoulder but refused to give me an MRI because the X-Ray looked fine. Yesterday I got the trembling while I was working on my computer. I’m about to start looking for a job and certainly would not want to have this hand seizures at work, or worse yet, at the interview…
Hello my name is Virginia. I had a shot in my butt in May 2018 and have had problems ever since then. I can tell it`s the nerve, it burns and hurts all the time. I went to a Chiropractic Dr. and that did not help. I`m loosing time from work, I can not do anything. Could you please refer me to a lawyer who is not scared of the Dr`s?
Hello Virginia, kindly see a physiotherapist as well to help reduce the pain and promote healing
I have been given a bad injection. I talked to a couple lawyers. They seem to not want the case because they can’t get rich off it. Do you know who I can contact about this?
Hello, I too would like the names of the medical doctors and lawyers that Maria mentioned. Thank you.
I took great intrest in all the comments made and bad experence everyone has to shear. I have kinda been in the situation myself. This was not related to any vaccine. In 1979 I was at the age of 22yrs and very pregnant. What really annoyed me was when they gave me a so call pain relief in my right thigh to carlm my contractions down, only to end up hitting the nerv, I live with this everyday since then, with nothing but pain 24/7 and was told that it will
NEVER HEAL. I was not even aloud to claim ACC back then and still Caint,to this day. How much longer do you have to suffer.
Have you heard of SIRVA VACCINES COMPENSATION?
In our case a student reported to have numbness over the injected site following Analgesic ,The case was reported after four months of injection.Is it possible to give a reply on this delayed response
Watch for Botox injections for pain. Sometimes you even don’t need it, but there is a botox scam out there. I had one in my arm, and am alarmed with the hand seizures I have in the mornings, and the deep pain I’m getting 3.5 months after I got the left arm injection. My doctor refuses to give me an MRI, saying, “it sounds like a nerve damage” but what can you do? What is done is done, and you can’t sue them because you signed a consent/release form.
I cannot believe that if this was from a vaccination, either flu, or anything considered a “vaccine”, then there would be resources, to go after the doctor who injured you.
My sister is in pain ever since she was injected in a vessels nothing is helping her leg…She is in and out of hospital without geting any help.
On Nov 1, 2018 I recieved a depo shot to my upper left shoulder. As soon as the needle entered my skin I knew something went wrong, it was so painful I jumped. After the nurse was done administering my entire left shoulder was throbbing in pain and started to spread to by back shoulder blade as well. The nurse told me to take ibprofin. In the days to follow:
4 days of throbbing shoulder pain
Sleepless night due to pain
electric shocks that ran from my elbow to my wrist
I can’t make a fist to painful
Hand and fingers are stiff and painful
Extreme painful tingles in my finger at times I have to constantly massage my had due to pain
Wrist pain as if I got instant carpal tunnel from the injection
I’m in pain all day till night feels like nerve damage.
It’s now nov 16, 2018 and heading to the dr for test on monday
I had a flu shot on the 2nd October which was administered by a very young Nurse (it is usually given by my GP) Since then I have had numbness and tingling down my arm and into my hand and sometimes it radiates down my leg. I have told my GP about this but getting nowhere. Taking this much further now.
Hi Laura! I’ve been experiencing same symptoms in my left arm and hand and yes, it began after I got the flu shot…and it didn’t help that I had another shot in the same arm, after being taken to ER due spinal issues. I appreciated your post…I’m curious to know what you mean by you’re “taking this much further now”. This is truly upsetting to me as I suffer from degenerative disc disease (my issues are in the lumbar spine) and yet I never had problems with my arms and hands until I got the flu shot and a muscle relaxant shot back in October this year. I also had a lumbar spine epidural injection this Monday…the left arm had been bothering me already but numbness and tingling of left arm and hand began after I went through the epidural this Monday. Already called my pain management doc to report these rather scary to me symptoms. Thank you and I hope you’re feeling better and your numbness and tingling has subsided.
It’s been almost 6 months since I’ve had a trigger point injection of Depo Medrol. It was put into 2 muscle groups with 80 mg. Pure hell. Anxiety, insomnia, weight loss, muscle pain, weakness, dry eyes & mouth, nerve issues. I have gone to so many doctors and physical therapy. I feel helpless. The only thing that has gotten better is my sleep. No lawyer will even touch this. It seems 80 mg was way too much to put into a 112 lb woman just into her trapezoid area. I can hardly work…
I have a chronic Illness that requires inpatient IV IM medication . I’ve been getting these treatments a few times a a month for over 8 yrs and have a IM injection everytime . I usually receive the injection of the same side and when it starts getting too numb I switch sides . Just a couple of weeks ago I had treatment and opted for the alternate side. The nurse obviously hit the nerve because I’ve been in pain ever since . I’m going to see my Primary Care Physician in a few days .
In 2000 in the USMC I was give a shot in left button by a navy corpsman and he hit the nerve so I jumped forward so he he rammed it further and and hooked it upwards. Immediatelly I started having problems and left hip pain. Shortly afterwards I started falling causing 4 dislocations and back problems. And VA doctors have brushed me off and even told me that that shot couldn’t cause long term damage . Ive had pain every day since and some days it’s so severe I can’t get out the floor. Ive had a limp for years and a good day is pain level of 3 or 4. And the VA still is no help and now doctors don’t want to prescribe pain medicine because of this stupid war on pain meds by a bunch of people who have never known what pain is.
I had an injection in my arm and instantly i knew something wasn’t right. It felt like a hot rod was being injected into my arm. It have been aince nov 2018 and i still have severe pain ,numbness and loss of motion in my arm. I am a yoga teacher and it has caused problems when i teach. I have an appointment with a neurologist soon. I hope he can help me. Do any of you think I have a legal case ?
I received a tetanus shot in 2007 in my upper left arm. As soon as the needle was removed it felt like it was still inside my arm and left a strange mark on my skin. This uncomfortable feeling stayed with me for several years and the mark on my arm grew to be about dime size. I went in to have it checked and was referred to a dermatologist who biopsied it and it turned out to be skin cancer. That doctor burned the skin cancer and left an even uglier permanent scar on my arm. Keep in mind I have been feeling like that needle is still in my arm and it has been 12 years since the injection. Now I’m suffering from what feels like, nerve damage and my entire bicep feels bruised and I have a very sharp shooting pain ranging from my bicep to my forearm and down into my fingers.
I have spoken with 2 doctors and the dermatologist and they all told me it has nothing to do with the tetanus shot. It has gotten worse over the past 3 months and is very painful.
I had a flu shot on December 4, 2018 and afterwards I had a lump at the injection sight that was very painful. I cannot lift my arm up or towards my back. I have been in pain ever since. I cannot sleep at night. I have to take Tylenol for the pain. My daughter helps me with latching my bra and combing my hair. It has been 2 months and I still can’t bend my arm to my back. My doctor told me it is osteoarthritis and sent me to a physical therapist. I try to do the exercises, but it is too painful. The pain is now radiating to my neck and shoulder. The pain is more at the injection site. I know the nurse had to of hit a nerve. There has to be a way to file a lawsuit. They should know what they are doing.
I had a b12 sho in my upper buttocks something I do once a week for years since I am highly anemic. This last time I went in and it was new, and I mean brand new nurse. It’s been over a week since, and now I have shooting sharp pain all over my side hip and leg. Will this go away? Will it get worse? should I go to a regular doctor? and also seek an attorney? I shutter to think this will be a permanent feeling, everytime I lay down it feels like I am sitting on needles. Need advice TIA
I got an injection in my right hip on Tuesday and then on Thursday I had severe pains. It was like a stabbing electric shock that felt like fire. It is continous unless I take a pain pill. Do you know how long tjis will last. I am worried.
Hi Debra.. It’s been 2 months and 12 days since I received an injection on the left butt cheek..immediatelt after receiving the injection I felt pain and numbness kicking in..as the dats went by i couldn’t feel my toes ,they were numb.i wasn’t able to bend any of my toes or my knee..everything was stiff and would swell. I could not sleep because of leg pain,Back pain and pain in the butt..i began taking therapy and i now can bend my knees but I’m still not able to bend all of my toes and i cant rest my foot down die to lots of pain and swelling.it is also very tender.i have missed two months of school..but therapy is the best option
After an operation my husband needed to have an injection every day to prevent him from the blood clot. One day he injected a needle on to his right thigh and the next day he was not able to walk because it was very painful on the spot that he put the needle in. Now it is almost 3 weeks the pain is still there. Is anybody know what should he do to ease the pain or what type of doctor or treatment that can help
I received several injections at a hospital and it’s been several months since then but my skin on my buttocks where they injected still hurts. It hurts when I brush my hand over the skin and the pain intensifies in the shower. Also when I touch those parts it doesn’t feel like I’m touching my own skin so evidently the sensitivity of those areas is messed up. There’s absolutely no visible injury besides these uncomfortable sensations. For the longest time I couldn’t figure out the cause but I think this may be it.
I received a b-12 shot in my right arm 6 to 8 weeks ago and my arm is sore numbness and tingling around the injection site. What to do
I gave birth to my son in 1991 by c-section, i had sever pain after the anesthesia wear off and they kept injecting me with pain meds on my right leg every 4 hours one of the shots they put on my leg was the most painful shot i ever felt in my life! And right away after the shot i felt my right leg numb i thought it would go away with time but Now is 2019, 26 years later and my right upper leg still numb and painful when i touch it! 🙁
[email protected]
I have been putting up with chronic pain in my upper left arm and shoulder since recieving a second round of a shingles vaccine. I’m guessing some nerve damage. I have been able to relieve the ache occasionally using ibeprophem..in fact it seemed to have gone for about 3 months but the ache has recently returned. Worse at night as I want to sleep on the left side.
My real question is has anyone found a successful treatment for this kind of nerve damage?
I got a depo provera shot in my right butt in june 2019 can’t recal the date but immediately while stil at the doctors practice i started feeling numbness in my butt and right leg. I couldn’t walk my leg was feeling week. I told the doctor he said it could be nerve damage. The doctor was not the one who administered the injection, it was the nurse because he was at theatre and came in a bit late. But i remained at his practice waited to tell him when he arrived. Since then i have this pain tht never goes away. It’s like im always tired and in pain like an old person.
Got a B-12 shot in my upper right hip, total pain and swollen no clue what to do, it has only been 1 week, im so miserable!
I had some sort of injection (supposedly intramuscular) in my right thigh in the ER over a year ago and I am still in pain, I can’t hardly stand anything to touch the area and God forbid my dog jumps on me and hits my leg it causes extreme pain. I don’t know what to do about it, any suggestions?
I am a diabetic and require that I give myself shots 4 times a day. I’ve done it for six years. Two weeks ago, I was injecting myself on the thigh and must have hit a nerve, now I get constant pain on that side of the leg from top to bottom. It affect me most at night time–sleeping. I can’t stay in one position for more than 4 minutes without moving again, because of pain. So I can’t get a good night sleep. I do ok during the day because I’m standing up and constantly moving which takes away from the pain.
40yrs ago after an operation a Nurse was annoyed at Me because I asked for pain medication so She jabbed Me so hard the when the Day Nurse came on and checked Me out, She said WOW Who did that to You and when I turned to see My Hip area there was a bruise the size of Texas. For many years I have suffered pain on and off. It would last a week sometime and then disappear for about a year and then would flare up again. I wonder if there is a “Statute of Limitation” on this kind of Barbaric behavior. Probably not.